ENDOVENOUS THERMAL ABLATION (EVTA) OF VARICOSE VEINS
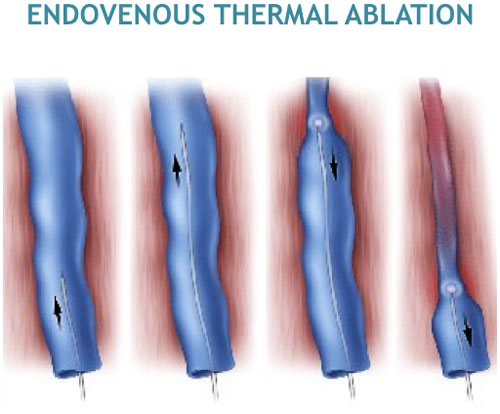
Endovenous Thermal Ablation (EVTA) of varicose veins?
This is a minimally invasive treatment for superficial venous reflux. In endovenous thermal ablation, there is no need for any groin incision or surgery. Instead, the vein remains in place and is closed using a special heating filament (laser fibre, radio frequency, steam etc.)
How is endovenous thermal ablation of varicose veins done?
A thin catheter (or wire) is inserted into the vein through a small needle puncture in the thigh or calf. A thin laser or radio frequency fibre is then passed up the catheter and activated. This imparts heat to the vein wall from within and causes it to collapse and close completely. This may eliminate the bruising and pain often associated with vein stripping that may result from the tearing of side branch veins while the saphenous vein is pulled out at stripping. The EVTA treated vein simply becomes fibrous tissue after treatment. Over time, the vein will gradually incorporate into surrounding tissue. This effectively works like actually opening up the limb and taking the vein out surgically, with the distinct advantage of much lesser incidence of vein regeneration and recurrence of varicose veins.
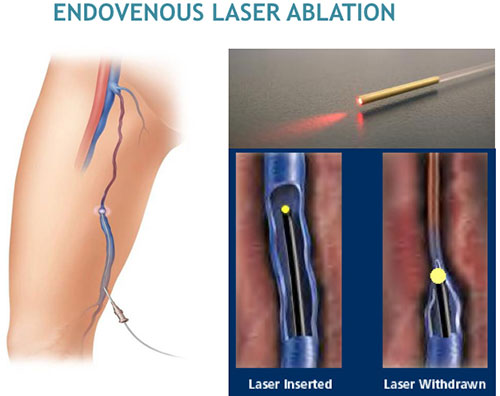
What is endovenous laser ablation (EVLA) of varicose veins?
Endovenous laser ablation or treatment (EVLA) is a minimally invasive ultrasound-guided technique used for treating varicose veins using laser energy. Laser fibers (with wave lengths varying from 810nm to 1470nm) are used to impart heat to the inner lining of the vein wall, resulting in its sealing off. The different wavelengths work on the water or hemoglobin respectively, thereby facilitating the vein to close and not allow blood to flow within. The laser fibre is activated and continuously withdrawn to impart 50-70 Joules/cm of heat energy to the vein.
What is Radio-frequency ablation (RFA) of varicose veins?
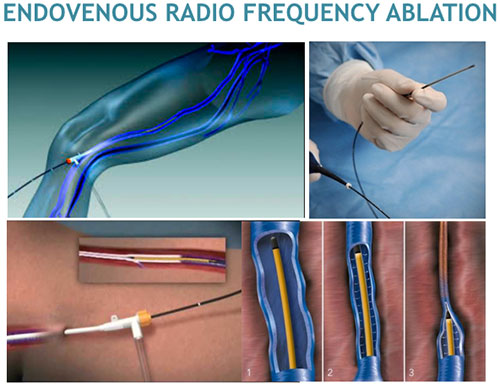
Radio frequency ablation is another popular form of endovenous thermal ablation of varicose veins, and is very similar to laser treatment. The main difference is the use of radio frequency waves (instead of laser) as the primary source of heat energy. Many believe that this causes less thermal collateral damage to the surrounding tissues (skin, fat, nerves). The radio-frequency electric waves (at 120oF)are given in pulses of 20 seconds per segment of vein, making it a quick and convenient method of ablation.
Does endovenous thermal ablation of varicose veins require anesthesia?
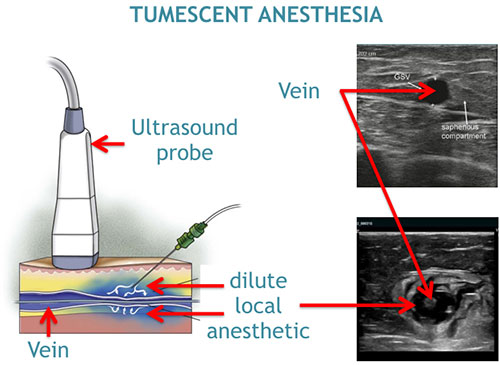
The procedure is performed on an outpatient basis or as day surgery, typically using local or regional anesthesia. Tumescent Anesthesia is a technique is which dilute local anesthesia is injected around and along the vein (perivascular infiltration) using ultrasound imaging. This allows the heat ablation to be carried out with the patient awake and also enables the patient to recover and get discharged a lot faster. Sometimes, your surgeon may offer you general anesthesia if multiple procedures are contemplated in the same sitting.
How long does endovenous thermal ablation of varicose veins take?
The procedure takes about 30-45min for each limb. If other procedures (e.g. Microphlebectomy, Sclerotherapy) are required, it may take longer.
What is the recovery after endovenous thermal ablation of varicose veins?

Most patients can resume normal activities immediately. For a few weeks (usually 2-3) following the treatment, your surgeon may recommend compression stockings and suggest you avoid very strenuous activities (e.g. heavy weight lifting) or prolonged periods of standing. There may be minimal to no scarring, bruising, or swelling lasting 1-2 weeks. Most patients report a noticeable improvement in their symptoms within a fortnight following the procedure.
What are the results and outcomes of endovenous thermal ablation of varicose veins?
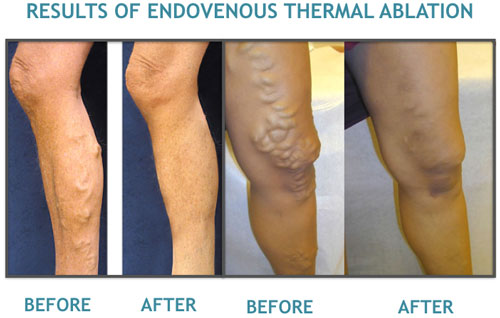
Published clinical data, with up to 5 years of follow-up, show success rates in excess of ninety percent of the EVTA-treated varicose veins remain closed and free from reflux, the underlying cause of varicose veins. This is much higher than surgical ligation and stripping and sclerotherapy. Over the last 10-15 years, EVTA has effectively replaced open surgical ligation and stripping as the primary modality of choice for the treatment of truncal varicose veins involving the long superficial veins of the lower limbs.
What are the complications of endovenous thermal ablation of varicose veins?
As with any medical intervention, potential risks and complications exist with the endovenous thermal treatment.
Severe bruising and pain may be experienced at the operated site. This is more common in patients on long-term blood thinners. It usually resolves in a few weeks.
The puncture site may have severe pain and an oozing of fluid from it, suggesting inflammation of the vein (thrombophlebitis). If pus oozes, it suggests a more serious infection and it is recommended to visit your surgeon immediately.
The skin and nerves near the vein can be burnt if the energy settings are high, or if the local (tumescent) anesthesia is not properly administered.
A clot may develop in the deep system of veins (deep vein thrombosis), though this is uncommon if the protocols are properly followed. It is associated with a hard swollen limb and has the risk of the clot dislodging and flowing to the heart and subsequently lungs (pulmonary embolism). This requires prompt diagnosis and management for a good recovery and outcome.
The procedure is now done safely all over the world, usually as an outpatient setting or day care with minimal complications. The techniques are now refined to minimize any problems.