ventral-incisional-hernia FOR LAPAROSCOPY
What is a Ventral Hernia?
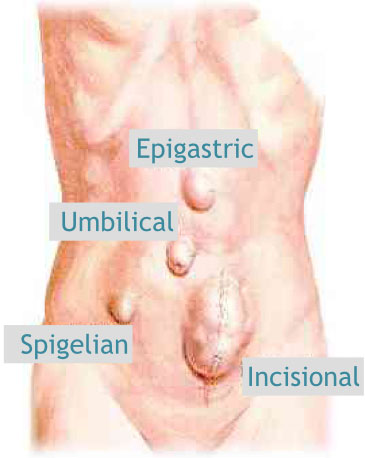
Ventral hernia is a term give for hernias through the anterior (front surface) abdominal wall (venter is Latin for belly). This will include Epigastric hernias (in the upper middle region of the abdomen), Paraumbilical hernias (all hernias in and around the belly button or umbilicus), Spigelian hernias (just outside the rectus muscle along its lower two-thirds), Lumbar hernia (in the lumbar region – outer flanks) and Incisional hernia (at the site of a previous surgical incision).They can occur spontaneously (primary hernia) or at the site of previous surgical incisions (secondary or incisional hernia).
Who can get a ventral hernia?

Men and women of all ages (including children and adults) can get hernias. It is more common in obese people, people with a weak abdominal tone, people who stain excessively and people with multiple abdominal surgeries etc.
Why does a ventral hernia occur?
Hernias occur through an area of weakness in the abdominal wall. This weakness may be congenital (present from birth) or acquired (occurring in later life) due to excessive strain on the abdominal wall from heavy lifting, weight gain, persistent coughing, or difficulty with bowel movements or urination. Factor like chronic illness, wasting, obesity, smoking and previous surgical incision etc., can predispose to the development of a hernia.
What are problems and complications of a ventral hernia?
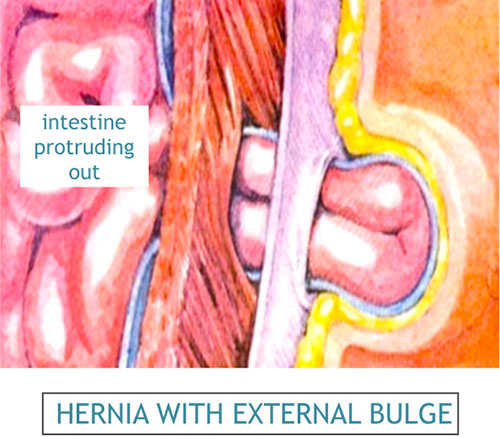
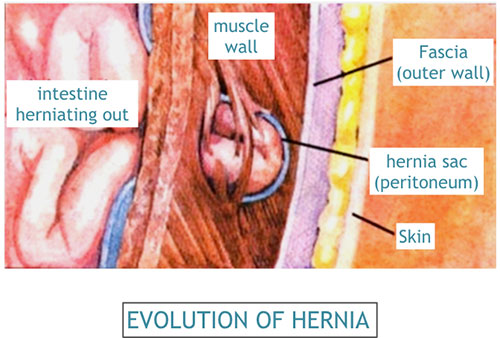
A hernia can progress through the various stages as it evolves. There is usually a weakness or tear at a point of the abdominal wall, where the abdominal contents try to push against the lining, forming a hernial sac. The contents gradually push open and spread the defect, making it bigger. The contents ultimately come out fully and can be seen as a swelling or bulge below the skin. The swelling usually becomes more prominent on coughing or straining (cough impulse). The hernial sac contents usually get emptied back into the abdominal cavity (reducible) and the swelling or bulge disappears.
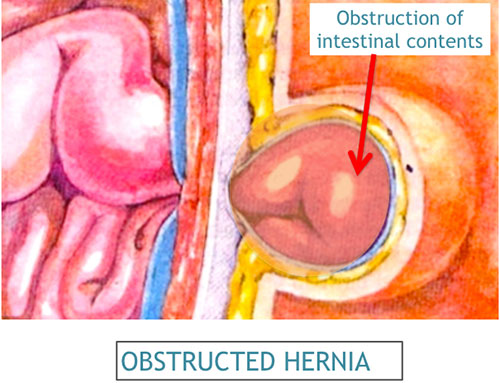
The abdominal muscles that form the margin of the defect can constrict the contents that pass through it, sometimes rendering these contents irreducible. Alternately, the contents of the sac can adherent to the lining of the hernial sac, which also results in the contents not being able to slide back inside. When a hernia involving the intestine is irreducible, it can block the flow of intestines, resulting in obstruction (blockage of smooth passage of gas, fluid or stools through the intestine) or incarceration (intestines in the hernial sac blocked with stools).

When the muscle contracts, it may constrict and actually cut off the blood supply to the intestines inside the hernial sac resulting in dead intestine (strangulation), which becomes an acute emergency. This gangrenous (dead) intestine can then tear open and spill inside, thereby contaminating the abdominal cavity.
What are the symptoms of a ventral hernia?

The symptoms listed below may accompany different hernias. Each person may experience different symptoms depending on the type of hernia and the individuals' physical health. A hernia specialist can properly diagnose your signs and symptoms and decide whether or not they are indeed related to a hernia.
Swelling or bulge on the abdominal wall:
The abdominal contents bulge out through an area of weakness through the abdominal wall causing a bulge. With strenuous activities such as lifting, straining or coughing the bulge tends to increase in size. A bulge may or may not be painful. However, even if the abnormal bulge is not painful it should never be ignored. It is best to seek opinion from a surgeon about it.
Pain or discomfort in the area of the bulge:
Patients with hernia often complain of pain, but all patients with hernia may not experience pain. When a muscle tears causing a hernia, a person may experience sudden pain followed by the appearance of a bulge. In some patients there may be no acute pain but merely a dull ache that usually subsides in a week or two. The hernia should not be ignored because the pain has gone away. The hernia will never go away, even if the pain has subsided. Some patients feel no pain but simply a funny feeling in the groin that they never had before. As a hernia enlarges, the surrounding nerves and tissues get stretched, resulting in more pain. Pain can also occur during activity such as exercise or strenuous work. This pain is a result of the hernial sac that contains lots of nerve endings getting pinched by the abdominal muscles during activity.
Pain in the entire abdomen:
Generalized pain all over the abdomen in a person who has a hernia is a serious symptom and should never be taken lightly. This type of generalized pain in the abdomen occurs with the hernia develops a complication like strangulation or incarceration. Often the bulge of hernia becomes prominent at the same time as the pain starts and does not go back in. This suggests that a part of intestine or other internal tissue may have got caught in the hernia and become pinched. As the blood supply of that tissue becomes compromised the person experiences severe pain. It may be accompanied by nausea or vomiting. This is a serious complication and the trapped tissues will die if surgery is not performed promptly.
Constipation:
Often a hernia develops because a person is constipated and has to strain while passing motion. Also, if the hernia is blocking the intestine you may experience constipation, or even blood in the stool.
How is a ventral hernia diagnosed?

A surgeon performs a thorough examination to diagnose a hernia and to determine its type. Some early or small hernias may require special tests (e.g. ultrasound or CT scan) to diagnose them. It is a good practice to image the entire abdomen for any associated pathology, which can be tackled simultaneously under the same anesthesia.
Can a ventral hernia be treated without an operation?
Without surgery, you must simply tolerate the hernia. A hernia once formed will never go away or become smaller on its own. Wearing a truss or binder may temporarily control the bulge from increasing in size, but it will not permanently cure the hernia. Surgery is the only permanent treatment for a hernia.
How can a ventral hernia be repaired?
Hernias usually need to be surgically repaired to prevent intestinal damage and further complications. This surgery may be performed by an open repair (small incision over the area of the hernia) or by laparoscopic surgery (minimally invasive key hole surgery). Your surgeon will determine the best method of repair for you and tailor-make the procedure to best suit your requirements.
What is the goal of the ventral hernia operation?
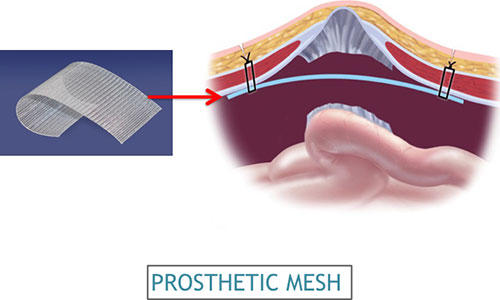
The main aim of the surgery is to push back all hernial contents and repair the defect, thereby to prevent any of the operations discussed earlier. The repair is usually done by a patch of prosthetic mesh (made of synthetic nylon), that reinforces the defective wall.
It is desired to have a pleasant hospital stay, a smooth operation, a quick and pain-free recovery and return to normal activity. It is important to minimize any chance of recurrence of the hernia as well long term discomfort in the groin area.
What happens before the ventral hernia operation?
Your surgeon will discuss the various types of operation and anesthesia available and then suggest what is best suitable to you. Before surgery, an evaluation of your general state of health, including a medical history and physical examination is performed. You will be asked to perform some routine investigations (blood tests, chest x-ray, ECG etc.). After your surgeon discusses all the potential risks and benefits of the operation, you will need to sign a written informed consent form for surgery.
The costing will be discussed with you, depending on the type (class) of hospital room you choose to stay in (e.g. general ward, twin-sharing, single, deluxe, suite etc.) and the choice of mesh. In case your medical insurance company or your employer is covering your medical expenses, you will have to get the necessary paperwork sorted out and sanctioned before admission.
Certain medicines such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) require to be stopped temporarily for 5-7 days prior to surgery, after consultation with your surgeon.
Quit smoking and arrange for any help you may need at home. Request a friend or relative to accompany you to hospital and take you home after discharge.
What anesthesia is used for a ventral hernia?
An abdominal wall hernia can be repaired under general, regional or local anesthesia. During the surgery, an anesthesiologist (a physician who specializes in anesthesia and pain relief) will recommend a type of anesthesia according to your condition and health status. Most ventral hernias are repaired under general anesthesia. You will not feel pain during the surgery.
What is involved in the ventral hernia operation?
You will be admitted on the morning of surgery (or on the previous night). You will be requested not to eat or drink anything for about 8 hours before surgery. The area to be operated upon may require to be shaved. It is recommended that you shower the night before and on the morning of the surgery. If you are constipated or have difficulties moving your bowels, an enema or laxative may be used after consulting with your surgeon. You will be given medications (e.g. antibiotics, pain killers etc.) during your hospital stay.
What are the different surgical options for ventral hernia?
Different methods of surgical methods are available for the repair of an abdominal wall hernia. The aim of all these methods is the same, but the approach differs, depending on whether it is performed by keyhole surgery (laparoscopy) or by conventional methods (open repair).
What is open repair of ventral hernia?
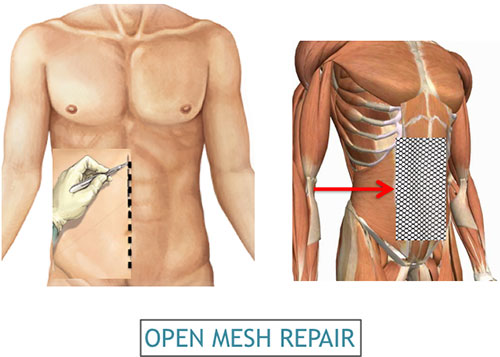
This procedure may be performed under general, regional or local anesthesia, depending on the hernia type and size, general condition and health. An incision or cut is made in the skin over hernia. The layers of the abdominal wall (including skin, fat and muscle) are opened to expose the hernia. The hernia “sac”, containing the bulging intestine or other contents, is identified. The surgeon pushes these contents inside the hernia sac back into its proper position behind the muscle wall. The muscle wall is reinforced with stitches or synthetic mesh to complete the repair. The abdominal wall layers are then closed appropriately. Most open hernia repairs require one or more drainage tubes to be placed at the operated site. These tubes are connected to small plastic vacuum bottles that continuously suck out all the liquefied and melted fat in contact with the mesh. These may be required for 5-10 days to keep the area dry and allow proper healing.
Most patients will be able to go home 48-72 hours after surgery with the drain bottles (or alternatively, stay in hospital till the bottles are removed in 5-10 days). Typically, most patients feel fine within a few days after the surgery and resume normal eating habits and activities. Strenuous activity and exercise are restricted for 4 to 6 weeks after surgery.
What is laparoscopic repair of ventral hernia?
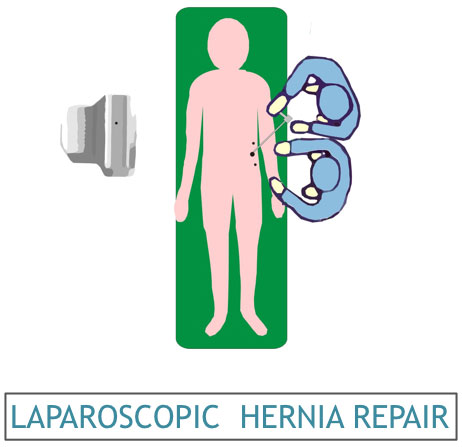
Usually, this procedure is performed under general anesthesia. Laparoscopic surgery uses a thin, telescope like instrument (known as an endoscope) that is inserted through a small incision on the abdominal wall. Usually, another two 5mm holes are required to allow other working instruments for the procedure. The endoscope is connected to a tiny video camera that projects an “inside view” of the patient’s body onto television screens in the operating room. The abdomen is inflated with a harmless gas (carbon dioxide) to allow your doctor to view your internal structures.
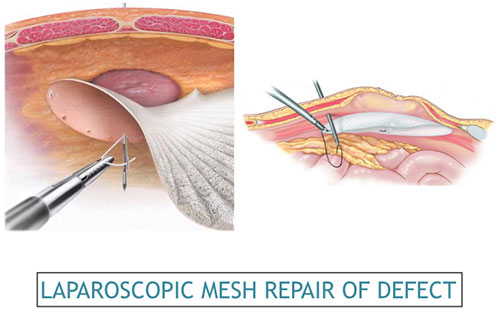
The hernial defects are identified and all its contents reduced. A laparoscopic view also allows us to detect and repair any other existing hernias that may have been missed on examination. A mesh patch is attached to secure the weak area and reinforce the defect. Following the procedure, the small abdominal incisions are closed with a stitch or two or with surgical tape. Within a few months, the incision is barely visible. The mesh that is used for laparoscopic surgery is made up of a specially coated material that does not react badly when in contact with the insides of the abdomen (especially the intestines) and is therefore more expensive that a mesh used for open hernia repair.
Most patients will be able to go home 24-48 hours after surgery. Typically, most patients feel fine a lot quicker than with open repair. Normal eating habits and activities (showering, driving, walking up stairs, lifting, working and engaging in sexual intercourse) can be resumed in a few days. Strenuous activity and exercise are restricted for 2 to 3 weeks after surgery.
In a small number of patients the laparoscopic repair cannot be performed. Factors that increase the possibility of choosing or converting to an "open" repair include obesity, a history of prior abdominal surgery causing dense scar tissue, inability to visualize structures or bleeding during surgery. The decision to choose or convert to the open repair is a decision made by your surgeon either before or during surgery. This is not considered a complication, but rather sound surgical judgment, strictly based on patient safety.
What are the advantages of having a laparoscopic ventral hernia operation?
- Three tiny scars rather than one larger incision
- Reduced postoperative pain
- Faster return to work
- Shorter recovery time and earlier resumption of daily activities (a recovery time of days instead of weeks)
- Lower Recurrence rates
- Lesser Complications
- Better ‘Patient Satisfaction’ and ‘Quality of life’ scores
What are the complications of the hernia operation?
Any surgical operation can be associated with complications. The primary complications of any operation are bleeding and infection, which are relatively less common with laparoscopic than with open hernia repair. There is a very small risk of injury to blood vessels, internal abdominal organs, urinary bladder or the intestines. A hernia that is surgically repaired can ‘come back’. Your surgeon will help you choose a procedure with a minimum risk of recurrence.
When to call your doctor after discharge from ventral hernia surgery?
It is important for you to recognize the early signs of possible complications. Be sure to call your physician or surgeon if you develop any of the following :
- Persistent fever
- Bleeding
- Purulent drainage (pus) from any incision
- Redness surrounding any of your incisions
- Increasing abdominal or groin swelling
- Pain that is not relieved by your medications
- Persistent nausea or vomiting
- Inability to pass urine
- Persistent cough or shortness of breath
- You are unable to eat or drink liquids