INGUINAL HERNIA
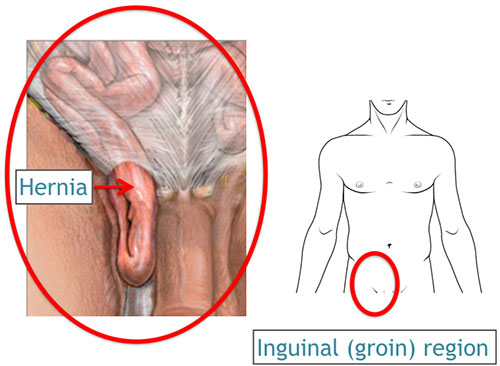
What is an inguinal hernia?
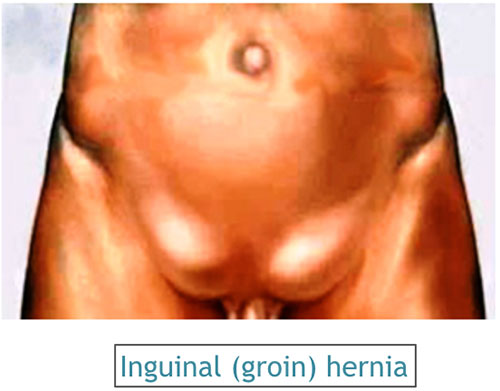
It is a weakness or tear in the abdominal muscles of the groin region, which allows the intestines, fatty tissue or an organ to protrude through this defect. The inner lining of the abdomen (peritoneum) pushes through the weakened area to form a sac. A loop of intestine or abdominal tissue can then slip into this sac causing pain and other potentially serious health problems.
Who can get an inguinal hernia?
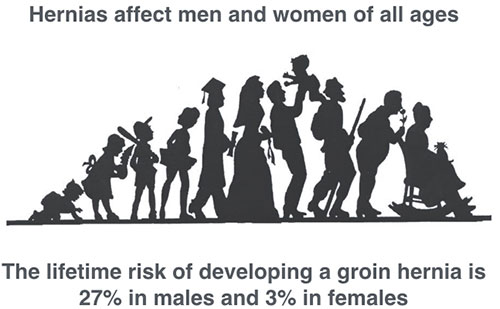
It is estimated that 20 million inguinal (groin) hernias are operated worldwide every year. Men and women of all ages (including children and adults) can get hernias. The lifetime risk of developing a groin hernia is 27% in males and 3% in females.
What causes an inguinal hernia?
Hernias occur through an area of weakness in the abdominal wall. This weakness may be congenital (present from birth) or acquired (occurring in later life) due to excessive strain on the abdominal wall from heavy lifting, weight gain, persistent coughing, or difficulty with bowel movements or urination. Factor like chronic illness, wasting, obesity, smoking and previous surgical incision etc., can predispose to the development of a hernia.
Collagen is a protein that is found in muscles and is responsible for its strength and elasticity. It is now believed that hernias occur when there is collagen failure i.e. defective collagen in the muscles that allow herniation through it.
What are the problems and complications of an inguinal hernia?
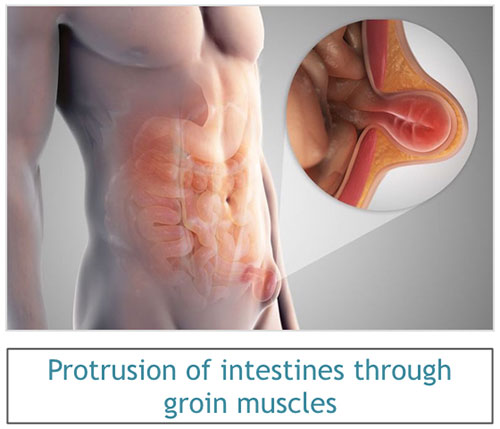
A hernia can progress through the various stages as it evolves. There is usually a weakness or tear at a point of the abdominal wall, where the abdominal contents try to push against the lining, forming a hernial sac. The contents gradually push open and spread the defect, making it bigger. The contents ultimately come out fully and can be seen as a swelling or bulge below the skin. The swelling usually becomes more prominent on coughing or straining (cough impulse). The hernial sac contents usually get emptied back into the abdominal cavity (reducible) and the swelling or bulge disappears.
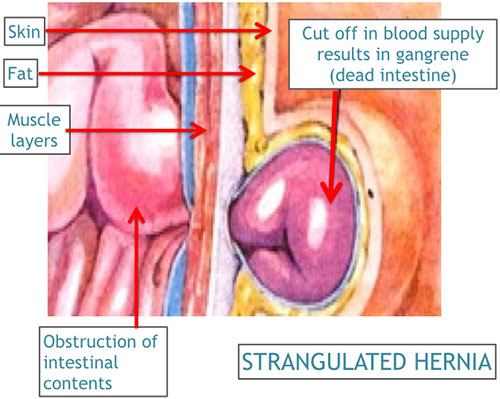
The abdominal muscles that form the margin of the defect can constrict the contents that pass through it, sometimes rendering these contents irreducible. Alternately, the contents of the sac can adherent to the lining of the hernial sac, which also results in the contents not being able to slide back inside (irreducible). When a hernia involving the intestine is irreducible, it can block the flow of intestines, resulting in blockage of smooth passage of gas, fluid or stools through the intestine (obstruction) or incarceration (intestines in the hernial sac blocked with stools).
When the muscle contracts, it may constrict and actually cut off the blood supply to the intestines inside the hernial sac resulting in dead intestine (strangulation), which becomes an acute emergency. This dead (gangrenous) intestine can then tear open and spill inside, thereby contaminating the abdominal cavity.
What are the symptoms of an inguinal hernia?

The symptoms listed below may accompany different hernias. Each person may experience different symptoms depending on the type of hernia and the individuals' physical health. A hernia specialist can properly diagnose your signs and symptoms and decide whether or not they are indeed related to a hernia.
Swelling or bulge beneath groin skin:
Laparoscopy is usually performed under general anesthesia, though in exceptional cases ‘diagnostic laparoscopy’ can be performed either under local anesthesia with sedation. With your help, your surgeon and an anesthesiologist will decide on a method of anesthesia to perform safe and successful surgery. General anesthesia is the usual choice for most patients undergoing laparoscopic surgery.
Pain or discomfort in the area of the bulge:
Patients with hernia often complain of pain, but all patients with hernia may not experience pain. When a muscle tears causing a hernia, a person may experience sudden pain followed by the appearance of a bulge. In some patients there may be no acute pain but merely a dull ache that usually subsides in a week or two. The hernia should not be ignored because the pain has gone away. The hernia will never go away, even if the pain has subsided. Some patients feel no pain but simply a funny feeling in the groin that they never had before. As a hernia enlarges, the surrounding nerves and tissues get stretched, resulting in more pain. Pain can also occur during activity such as exercise or strenuous work. This pain is a result of the hernial sac that contains lots of nerve endings getting pinched by the abdominal muscles during activity.
Pain in the entire abdomen:
Generalized pain all over the abdomen in a person who has a hernia is a serious symptom and should never be taken lightly. This type of generalized pain in the abdomen occurs with the hernia develops a complication like strangulation or incarceration. Often the bulge of hernia becomes prominent at the same time as the pain starts and does not go back in. This suggests that a part of intestine or other internal tissue may have got caught in the hernia and become pinched. As the blood supply of that tissue becomes compromised the person experiences severe pain. It may be accompanied by nausea or vomiting. This is a serious complication and the trapped tissues will die if surgery is not performed promptly.
Constipation:
Often a hernia develops because a person is constipated and has to strain while passing motion. Also, if the hernia is blocking the intestine you may experience constipation, or even blood in the stool.
Urinary difficulties:
If the bladder becomes trapped within the hernia, you may develop urinary burning, frequent infections or frequency in urinating. You should consult a surgeon if you are experiencing these symptoms so he can examine you to determine if a hernia is present. Also, patients with a prostate problem tend to develop hernias as a result of constant straining at the time of urination.
How is an inguinal hernia diagnosed?
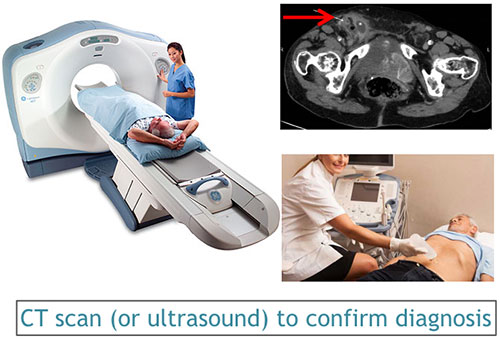
A surgeon performs a thorough examination to diagnose a hernia and to determine its type. Some early or small hernias may require special tests (e.g. ultrasound or CT scan) to diagnose them. These tests also help look for other abdominal diseases that may be picked up incidentally.
Can an inguinal hernia be treated without an operation?

Without surgery, you must simply tolerate the hernia. A hernia once formed will never go away or become smaller on its own. Wearing a truss or binder may temporarily control the bulge from increasing in size, but it will not permanently cure the hernia. Surgery is the only permanent treatment for a hernia.
How can an inguinal hernia be repaired?

Groin hernias usually need to be surgically repaired to prevent intestinal damage and further complications. This surgery may be performed by an open repair (small incision over the area of the hernia) or by laparoscopic surgery (minimally invasive key hole surgery). Your surgeon will determine the best method of repair for you and tailor-make the procedure to best suit your requirements.
What is the goal of the hernia operation?

The main aim of the surgery is to push back all hernial contents and repair the defect, thereby to prevent any of the complications discussed earlier. The repair is usually done with a patch of synthetic nylon (mesh) that reinforces the defective wall.
It is desired to have a pleasant hospital stay, a smooth operation, a quick and pain-free recovery and return to normal activity. It is important to minimize any chance of recurrence of the hernia as well long term discomfort in the groin area.
What happens before the hernia operation?
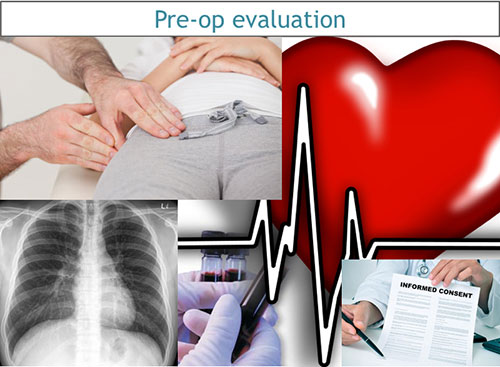
Your surgeon will discuss the various types of operation and anesthesia available and then suggest what is best suitable to you. Before surgery, an evaluation of your general state of health, including a medical history and physical examination is performed. You will be asked to perform some routine investigations (blood tests, chest x-ray, ECG, sonography etc.). After your surgeon discusses all the potential risks and benefits of the operation, you will need to sign a written informed consent form for surgery. The costing will be discussed with you, depending on the hospital room you choose to stay in (general/sharing/private). In case your medical insurance company or your employer is covering your medical expenses, you will have to get the necessary paperwork completed and approved before admission.
Certain medicines such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) require to be stopped temporarily for 3-5 days prior to surgery, after consultation with your surgeon. Quit smoking and arrange for any help you may need at home. Request a friend or relative to accompany you to hospital and take you home after discharge.
You will be admitted in hospital on the morning of surgery (or on the previous night). You will be requested not to eat or drink anything for about 6-8 hours before surgery. The area to be operated upon may require to be shaved. It is recommended that you shower the night before and on the morning of the surgery. If you are constipated or have difficulties moving your bowels, an enema or laxative may be used after consulting with your surgeon. You will be given medications (e.g. antibiotics, pain killers etc.) during your hospital stay.
What anesthesia is used for an inguinal hernia?

An inguinal hernia can be repaired under general, regional or local anesthesia. In general anesthesia, the patient is fully asleep and unaware of the surroundings. In regional anesthesia, the anesthetic agent is injected in the back (spinal block) to numb the lower half of the body. For local anesthesia, the groin region is injected with the numbing agent so that the patient cannot feel any pain during the procedure. He is usually awake and aware of he proceedings, though a mild sedative may be given to alleviate anxiety and help him sleep during the entire operation.
During the surgery, an anesthesiologist (a physician who specializes in anesthesia and pain relief) will recommend a type of anesthesia according to your condition and health status. You will not feel pain during the surgery.
What are the different surgical options for inguinal hernia?
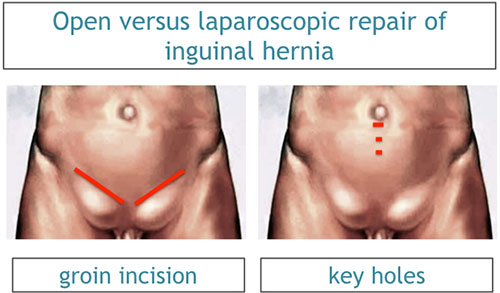
Different surgical methods are available for the repair of an inguinal hernia. The aim of all these methods is the same, but the approach differs, depending on whether it is performed by keyhole surgery (laparoscopic repair) or by conventional methods (open repair).
What is open repair of inguinal hernia?
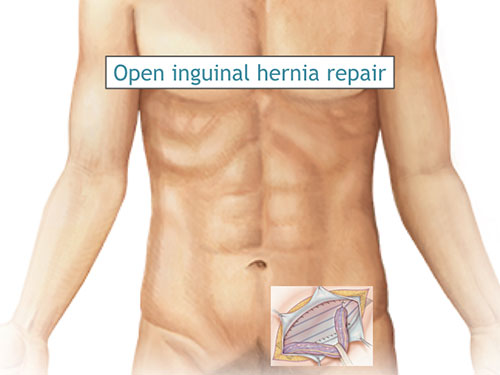
This procedure may be performed under general, regional or local anesthesia, depending on the hernia type and size, general condition and health. An incision or cut is made in the skin over in the groin area, measuring about 4-6cm in length. The layers of the abdominal wall (including skin, fat and muscle) are opened to expose the hernia. The hernia sac, containing the bulging intestine or other contents, is identified. The surgeon pushes these contents inside the hernia sac back into its proper position behind the muscle wall. The muscle wall is reinforced with stitches or synthetic mesh to complete the repair. The abdominal wall layers are then closed appropriately.
Most patients will be able to go home 24 hours after surgery. Typically, most patients feel fine within a few days after the surgery and resume normal eating habits and activities. Strenuous activity and exercise are restricted for 4 to 6 weeks after surgery.
The open repair is a popular choice when the inguinal hernia is large, irreducible, obstructed or strangulated, or when local anesthesia is preferred in lieu of age or other existing medical problems that may worsen with general anesthesia.
What is laparoscopic repair of inguinal hernia?
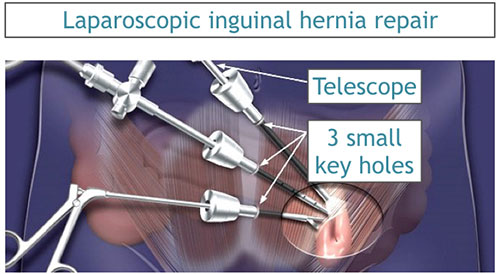
Usually, this procedure is performed under general anesthesia. Laparoscopic surgery uses a thin telescope (laparoscope) that is inserted through a small incision below the umbilicus (belly button). The telescope is connected to a high definition video camera that projects the inside view of the patient’s body on to television screens in the operating room. The abdomen is inflated with a gas (carbon dioxide) to allow your doctor to view the internal structures. The hernial defects are identified and all its contents reduced. A laparoscopic view also allows us to detect and repair any other existing hernias (e.g. femoral, obturator etc.) in the groin. A prosthetic mesh is deployed to secure the weak area and reinforce the defect. Following the procedure, the small abdominal incisions are closed with a stitch or two or with surgical tape. Within a few months, the incisions are barely visible.
Most patients will be able to go home 24 hours after surgery. Typically, most patients feel fine a lot quicker than with open repair. Normal eating habits and activities (showering, driving, walking up stairs, lifting, working and engaging in sexual intercourse) can be resumed in a few days. Strenuous activity and exercise are restricted for 2 to 3 weeks after surgery.
Laparoscopic repair is a popular choice in patients who are fit for general anesthesia, have uncomplicated hernias, recurrent hernias and those who have bilateral hernias or a suspicion of a defect on the opposite side.
In a small number of patients the laparoscopic repair cannot be performed. Factors that increase the possibility of electively choosing or converting to an "open" repair include obesity, a history of prior abdominal surgery causing dense scar tissue, inability to visualize structures or bleeding during surgery. The decision to choose or convert to the open repair is a decision made by your surgeon either before or during surgery. This is not considered a complication, but rather sound surgical judgment, strictly based on patient safety.
What are the advantages of having a laparoscopic operation?

- Three tiny scars rather than one larger incision
- Reduced postoperative pain
- Faster return to work
- Shorter recovery time and earlier resumption of daily activities (a recovery time of days instead of weeks)
What are the complications of the operation?

Any surgical operation can be associated with complications. The primary complications of any operation are bleeding and infection, which are relatively less common with laparoscopic than with open hernia repair. There is a very small risk of injury to blood vessels, nerves or the spermatic tube, urinary bladder or the intestines. Difficulty in urinating can occur after surgery and may even require a temporary tube (catheter) into the urinary bladder.
A hernia that is surgically repaired can come back. Your surgeon will help you choose a procedure with a minimum risk of recurrence.
When to call your doctor after discharge from inguinal hernia surgery?

It is important for you to recognize the early signs of possible complications. Please contact your surgeon if you have any of the following:
- Persistent fever
- Bleeding
- Purulent drainage (pus) from any incision
- Redness surrounding any of your incisions
- Increasing abdominal or groin swelling
- Pain that is not relieved by your medications
- Persistent nausea or vomiting
- Inability to pass urine
- Persistent cough or shortness of breath
- You are unable to eat or drink liquids