PERIANAL ABSCESS
What is a perianal abscess?
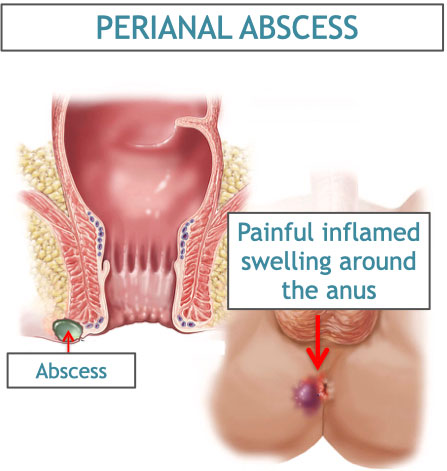
Perianal abscess is a collection of pus near the anal region. It is a common condition and can be very distressing. It is associated with pain, swelling and discharge near the anal region.
How does it occur?
With constipation, a hard bowel movement can erode the lining in the anal canal, resulting in infections of small glands in the anal lining. This results in swelling and formation of pus that increases to a significant size. Eventually, the pus finds its way through or around the sphincter muscles of the anus and out through the skin around the anus or internally.
The following factors can increase the likelihood of developing a fistula:
- straining to have a bowel movement when you are constipated
- waiting too long to have a bowel movement
- having less fibre in diet
- insufficient water intake
- low immunity states: diabetes, steroid intake, other diseases.
What are the symptoms of a perianal abscess?
Symptoms of perianal abscess include:
- pain and swelling near the anal region
- pus discharge after an episode of intense pain
- fever
- a swelling noted around the anus
- sometimes a sensation of “internal pain” or itchiness in the region may indicate the presence of perianal abscess
How is a perianal abscess diagnosed?
Your health care provider will examine your rectum and anus. It may be a little painful if there is a swelling/ recent pain/pus discharge. Proctoscopy (examination with a small instrument) may be performed using a local anaesthetic ointment, to better assess the anal region. An MRI of the perianal region may be performed, to identify the size, extent and connections of the abscess.
What are the different types of perianal abscess?
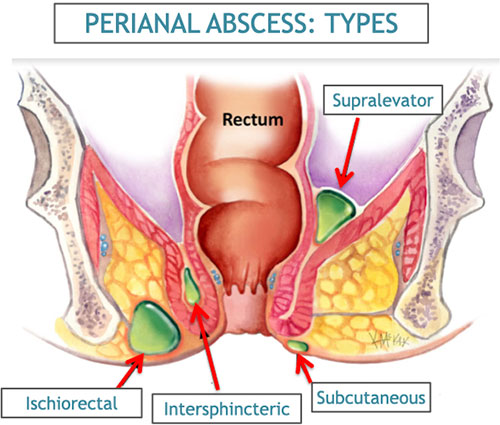
There are different types of perianal abscesses. based on their location around the anal region:
Submucosal- usually felt from within by the doctor
Intersphincteric- within the muscle layers in the anal region
Extrasphincteric- just outside the muscle layers in the anal region
Ischiorectal- spreading in the surrounding region
Subcutaneous- spreading under the skin around the anal region
or a combination of any of these.
A horseshoe perianal abscess is one that has spread from one side to the other, almost enveloping the anal region, like a U-bend or a horseshoe.
How is a perianal abscess treated?
Surgery is the only definitive treatment for perianal abscess. In some cases, if the abscess has already burst and there is no significant pus collection left within, your healthcare provider may consider giving you a simple trial of antibiotics without surgery. However, it is not advisable to wait by yourself for the abscess to burst, as that has a very high risk of fistula formation and slower recovery, due to inner pus collections that may be left untreated.
What are the surgical options for perianal abscess?

Classically, the painful perianal abscess had painful surgical options:
- Cruciate incision, drainage and debridement, which often leaves a large scar
- Deroofing, incision and debridement of perianal abscess wall, which has a high risk of incontinence, and a large scar.
Today, we are able to provide better surgical treatment options for perianal abscess:
- Small incision, flushing and debridement, with a small temporary drain pavement in the abscess cavity
- Laser ablation of abscess wall and debridement, through a 10mm incision near the anal region.
The newer techniques with smaller incision allows for quick healing of the wound and recovery in 2-3 weeks. The chances of fistula are less with laser ablation, and the risk of incontinence is negligible.
What are the other treatment/ supportive care should i take for perianal abscess?
High-fibre diet
Eat more high-fibre foods, which will help prevent constipation. Good sources of fibre include fresh fruit; raw or cooked vegetables, especially asparagus, cabbage, carrots, corn, and broccoli; and whole-grain cereals with bran, such as shredded wheat or bran flakes.
Fluids
Drink plenty of water. This helps to soften stools so they are easier to pass.
Sitz baths and cold packs
Sitting in lukewarm water 2 or 3 times a day for 15 minutes cleans the anal area and may relieve discomfort. Also, you might try putting a cloth-covered ice pack on the anus for 10 minutes, 4 times a day.
Medications
Antibiotics are needed if there is active pus discharge, to reduce the infection. They are also used during and after the surgery, so as to control any infection. Local anaesthetic and disinfectant creams along with a stool softener and an oral painkiller are also prescribed.
How long will the effects last?
In most cases the symptoms go away in a few days after surgery. The wounds in more severe cases should get better in a couple of weeks. A wound check and clean up may be required after 3-4 days of surgery, especially in large abscesses.
How can I take care of myself?
Always tell your health care provider when you have anal pus discharge, pain or fever. Although a few drops of blood/ fluid is expected after fistula surgery.
Follow these guidelines to help prevent fistulas and to relieve their discomfort:
- Do not strain during bowel movements. This only increases the force of injury.
- Follow your high-fibre diet and drink plenty of water. If necessary, take a stool softener. Softer stools make it easier to empty the bowels and reduce pressure on the veins.
- Don't overuse laxatives. Diarrhea can be as damaging to the anus as constipation.
- Ask your health care provider what nonprescription product you should buy to relieve pain and itching. Also, ask about any side effects of any medications prescribed for you.
- Exercise regularly to help prevent constipation.